
Humans and other animals have evolved adaptations to hypoxia, most famously among high altitude people. Oxygen availability, especially at the tissue level, varies at sea level too. Adaptation to hypoxic stress is important in wound healing, defense against infection, and protection from sepsis.
Hypoxia stimulated HIF-1α has a key role in tissue recovery, protective inflammation, and neuroprotection HIF-1α stimulates angiogenesis and promotes tissue repair after traumatic brain injury. Recovery from wounds involves adaptation to hypoxic stress by HIF-1α signaling. After trauma and burns, HIF-1 appears to protect the host by preventing infection and sepsis. The mechanism of protection from infection by HIF-1α includes activation of inflammation and increased bacterial killing by myeloid cells. Peyssonnaux et al. (2005) showed that mice with inhibited HIF-1α showed “decreased bactericidal activity and failed to restrict systemic spread of infection from an initial tissue focus.” Conversely, when they activated HIF-1α pathway through deletion of von Hippel-Lindau tumor-suppressor protein the mice showed improved antibacterial defenses and bacterial killing by phagocytes. HIF-1α activation also reinforces the intestinal epithelial barrier during sepsis. Hypobaric hypoxia activates similar inflammatory pathways, mediated by the toll-like receptor TLR4 and HIF-1. These shared mechanisms may explain why altitude illnesses have similarities with sepsis as we pointed out recently.
McKenna and colleagues made a similar argument, noting that adaptation to hypoxia might have a beneficial role in recovery from sepsis. During critical illness, they propose that organ dysfunction could be “an evolutionarily conserved strategy of cellular reprogramming to limit damage during hypoxic stress.”
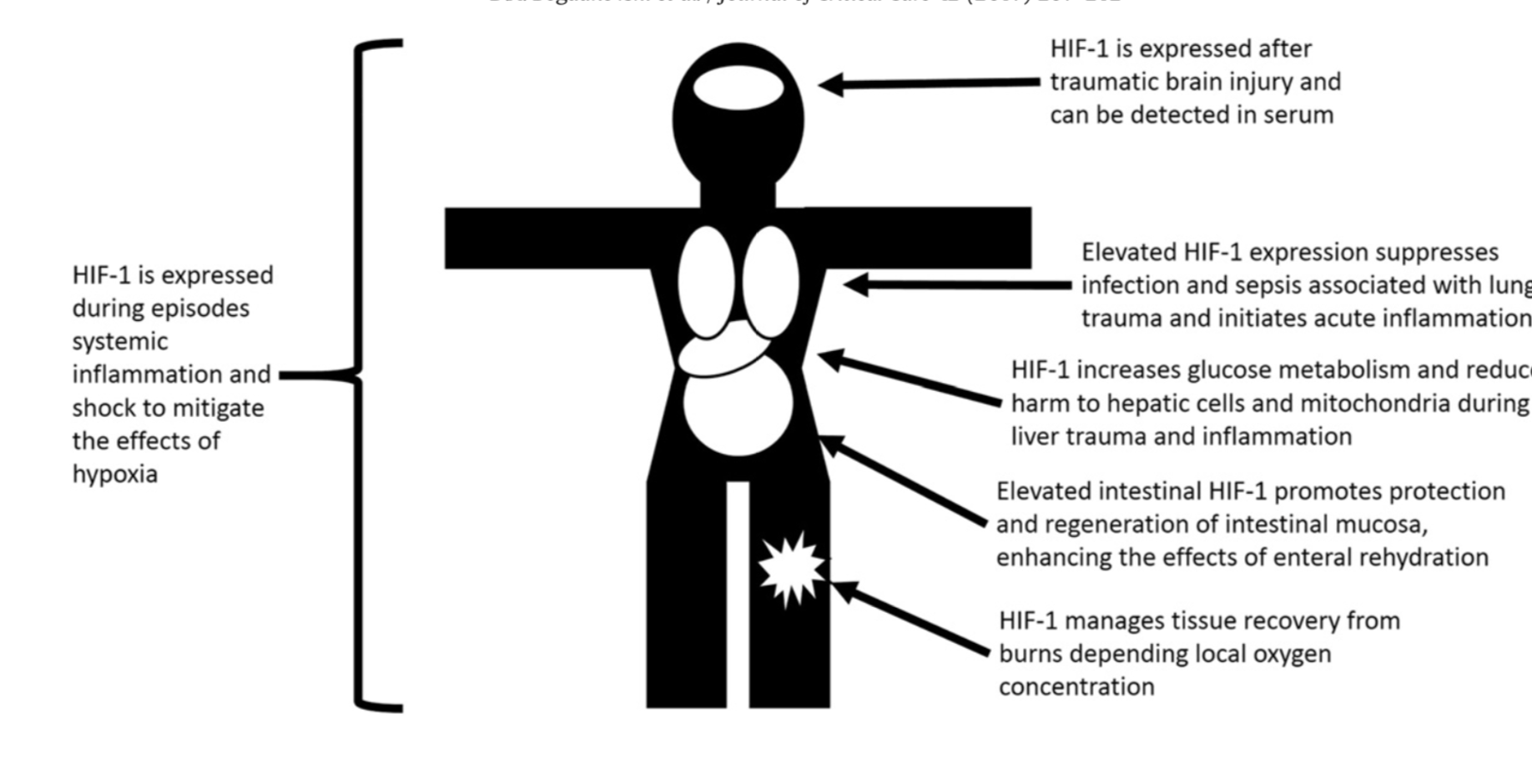
These findings – showing that HIF-1α is important in recovery from infection, injury and sepsis – lead to questions about using too much oxygen in the ICU. Could supplemental oxygen interfere with the evolved role of HIFs in infections – e.g. urinary tract infections – and injury – e.g. traumatic brain injury?
Mervyn Singer and colleagues warned that we harm patients when oxygen tension is higher than normal. A key concern is heightened oxidative stress. Hyperoxia causes increased reactive oxygen species, harmful vasoconstriction and vasodilation, DNA damage, and pulmonary epithelial injury. These proximate mechanisms are illustrated below:

An influential meta-analysis of observational and randomized trials of oxygen, the IOTA study, raised concern about increased mortality from excess oxygen in patients with heart attacks, strokes, and in the intensive care unit. We wrote and podcasted about IOTA here and here. Since then, a raft of randomized trials comparing liberal versus conservative oxygen have been published. The results are mixed. A 2023 Cochrane review comparing higher versus lower targets of arterial oxygenation in ICU patients concluded that for all trials, no significant difference for mortality between the two strategies (risk ratio (RR) 1.01, 95% confidence interval (C)I 0.96 to 1.06.
Sepsis might be a different story. From the Cochrane review: “Meta‐analysis of all trials indicated harm from higher oxygenation strategies as compared with lower on the occurrence of sepsis at maximum follow‐up (RR 1.85, 95% CI 1.17 to 2.93; I2 = 0%; 752 participants; 3 trials; very low‐certainty evidence).”
I have seen one major change in how we use oxygen. When I began my career we routinely gave supplemental oxygen to patients with acute myocardial infarctions (heart attacks). In practice this meant that anyone with chest pain in the ER was given oxygen by protocol. After early studies suggested harm, questions were raised about this practice. A 2017 NEJM study randomized 6629 patients with suspected myocardial infarction to either air or oxygen, which was delivered by facemask at 6 L/minute. This study found no benefit for mortality, rehospitalization or repeat acute myocardial infarction – to those given oxygen. Since these results, we have dropped oxygen as routine therapy for our chest pain patients.
This year two important trials were published, each testing the practice of conservative oxygen therapy in critically ill adult patients. Both showed no improvement in mortality from a conservative oxygen strategy- although both concluded that the practice was safe. In other words, limiting oxygen doesn’t increase the rates of death or significant adverse events.
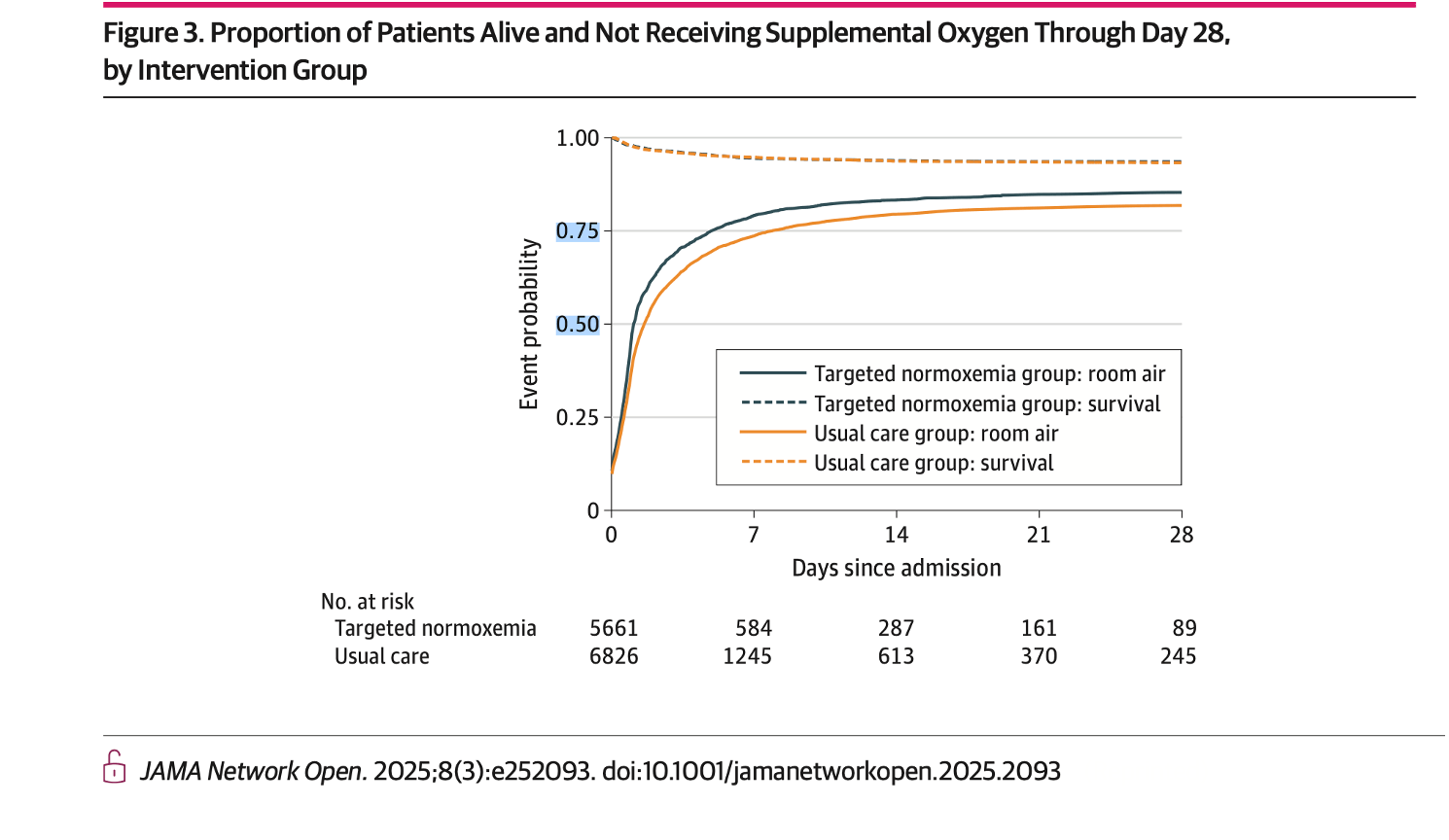
The first study involved trauma patients admitted to the ICU. Douin and colleagues studied the effect of decreasing the supplemental oxygen administered whenever SpO2 exceeded 96% using a cluster RCT design. They enrolled 12,000 trauma patients and found that the intervention was safe but had no impact on mortality or recovery overall. Separately, Douin reported a benefit of targeted normoxemia in the subset of patients with traumatic brain injury, but that promising clue will need to be followed up with another prospective trial.
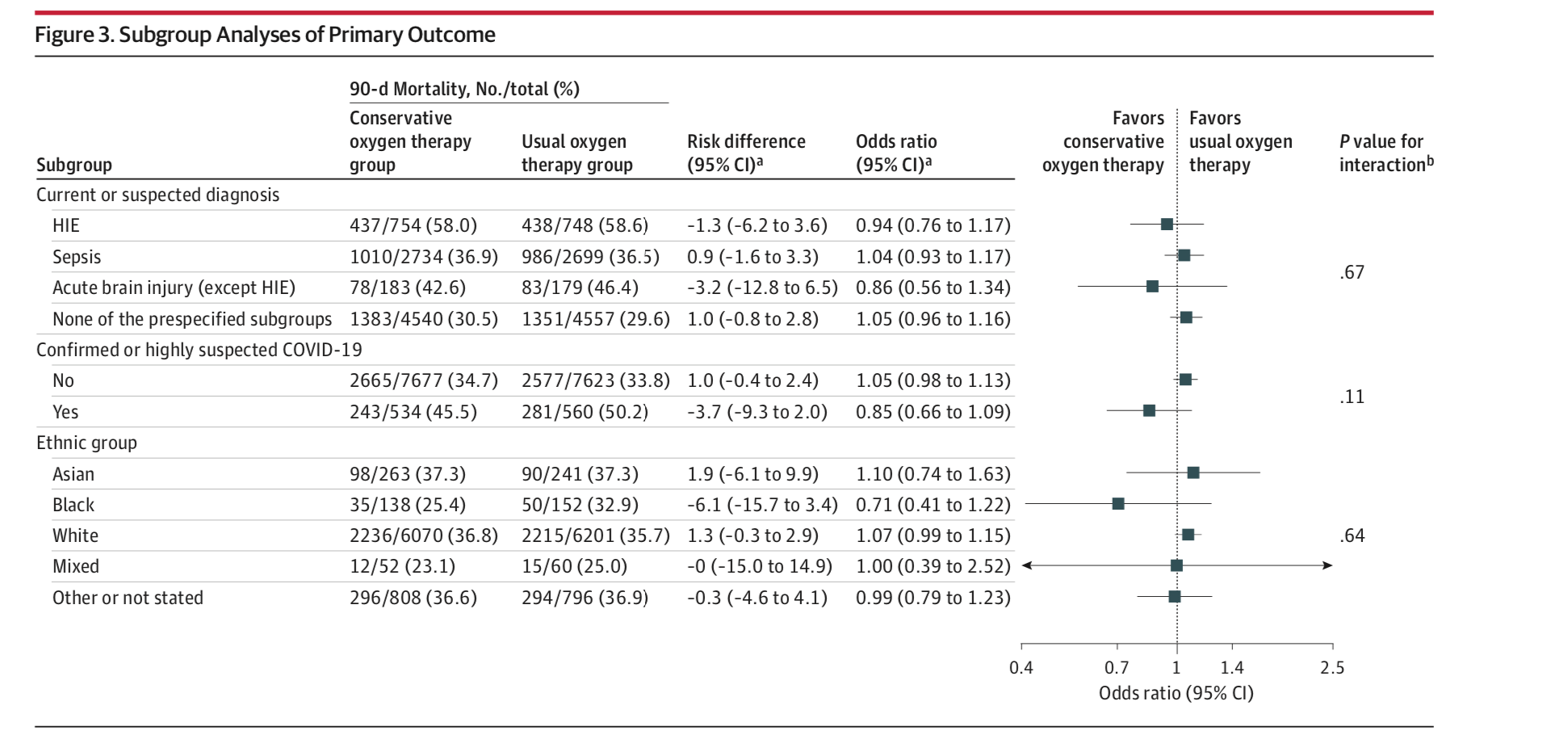
The second trial from the UK randomized 16,500 mechanically ventilated adults to a conservative oxygen target versus usual care with no upper limit of oxygen. The conservative oxygen target group were maintained with an oxygen saturation of peripheral oxygen [SpO2] target, 88%–92%) versus usual care (no upper-limit target). The primary outcome – 90-day mortality – was not significantly different between two groups. Oxygen limitation had no effect on outcomes in sepsis and brain injured subgroups.
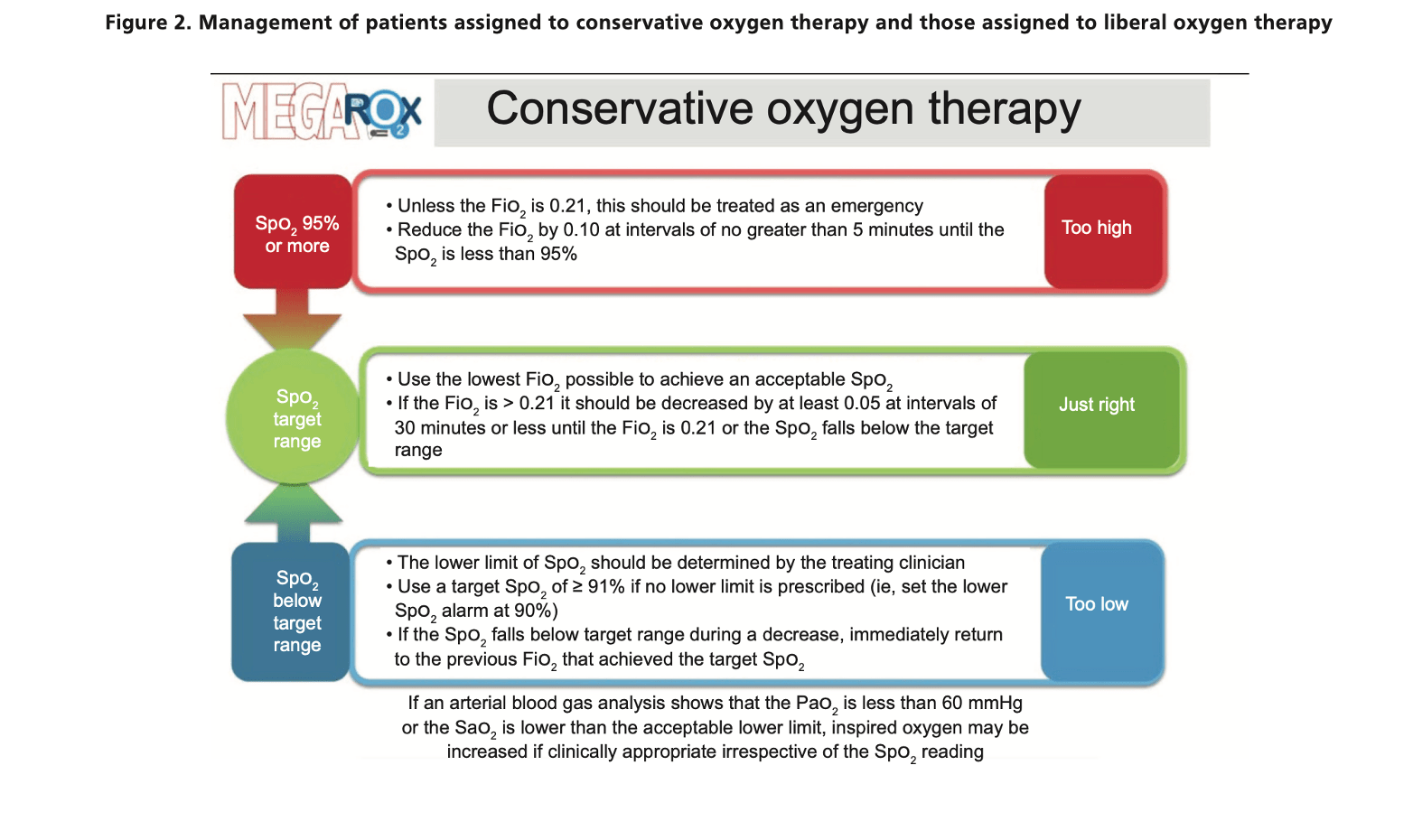
This null result surprised many who have been following this literature. It is noteworthy that the two groups had relatively small differences in oxygen saturation, suggesting that clinicians are already aware of the potential harm of excessively high oxygenation. The final word on the topic will have to wait for the results of the MegaROX trial, a study of 40,000 hospitalized patients:
Until then, limiting oxygen appears to be safe, but not necessarily life saving. This conclusion is consistent with an evolved role for HIF in buffering our bodies from the microbial, energetic and oxidative stresses of hypoxia.
Categories: Uncategorized
Joe Alcock
Emergency Physician, Educator, Researcher, interested in the microbiome, evolution, and medicine
Leave a comment