Is it normal to be hypoxic in the earliest stages of life? Maltepe and Saugstad 2009 write: “It is known that oxygen levels are low in fetal life with saturations as low as 50% or even lower. After birth, arterial oxygen saturation increases slowly and reaches 90% with a median time of 5 minutes in normal healthy babies. However, levels as low as 40% are reported in normal newborn babies during the first 3–4 min of life.”
Since term newborns tolerate oxygen saturations as low as 40% in the first 5 minutes of life, perhaps some oxygen therapy is needless or excessive. Exposing newborns to excess oxygen in sensitive periods of development has been shown to have harmful long term consequences. For babies born at term, a recent meta-analysis showed that 100% oxygen resulted in higher mortality compared to resuscitation with air (21% O2). In premature infants, retinopathy of prematurity (ROP) and bronchopulmonary dysplasia (BPD) are two well-documented complications of oxygen therapy. The problem is: how should we proceed when neonates need oxygen?
Maltepe and Saugstad wrote: “Importantly, the biologic defenses against hyperoxia may not be as robust as against hypoxia given that during evolution no organisms would have been exposed to supraphysiological oxygen tensions.” This perspective suggests that we risk complications when giving 100% oxygen owing to a gene-environment mismatch.
While we lack adaptations to 100% oxygen, it is worth pointing out that our distant evolutionary ancestors were once exposed to higher concentrations. Oxygen concentration in the late Carboniferous and early Permian period may have reached levels as high as 35%.
There is never a perfect concordance between our genes and the environment we inhabit. Natural selection tends to make individuals more fit over generations to various features of the environment, but because of constant change, our genes and our bodies are never perfectly adapted. Selection shaped our genomes according to the logic of a bygone environment (the environment of evolutionary adaptedness or EEA). This discordance explains problems caused by evolutionary novelties, like breathing 100% oxygen.
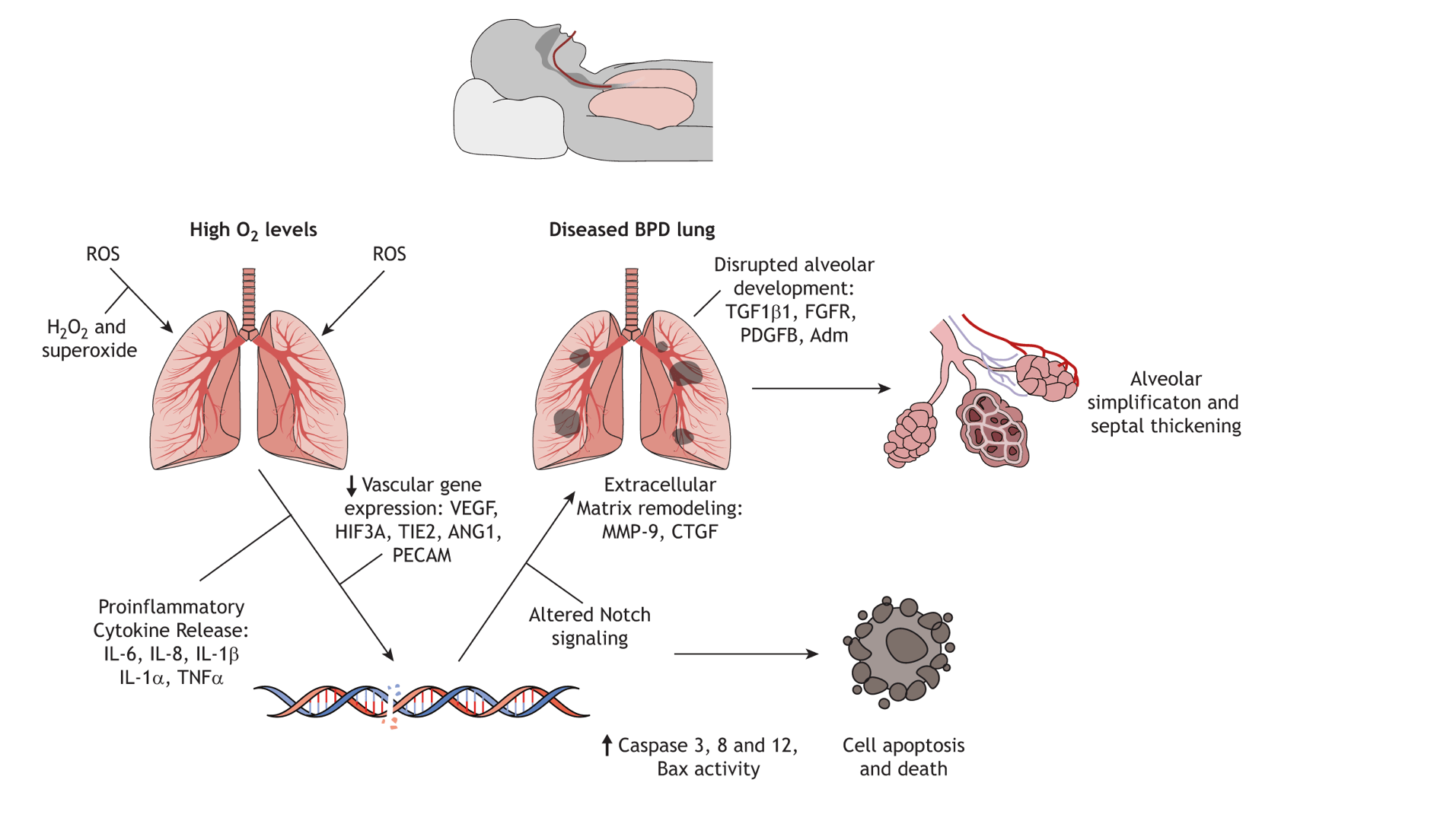
Premature infants especially have high oxygen requirements since their immature lungs lack surfactant and cannot take up oxygen efficiently. These babies need high O2 at a stage of life when oxygen regulates blood vessel development. Unfortunately this leads to bronchopulmonary dysplasia (BPD), and retinopathy of prematurity (ROP) as a consequence of high O2. These problems result from suppression of hypoxia inducible factors that regulate alveolar and vascular development – a classic gene-environment mismatch.
To avoid these developmental complications, a variety of studies have tested whether we can safely reduce the amount of oxygen in the neonatal ICU. To date there have been 5 randomized controlled trials of targeting a lower oxygen saturation (85%-89%) compared with a higher saturation (91%-95%) in very premature infants. Permissive hypoxia groups had less ROP and BPD. However in 3 of the 5 studies mortality was higher in the lower oxygen targets. The more hypoxic group also tended to have more necrotizing enterocolitis (NEC), catastrophic disease in which segments of the gut become ischemic and die. Clearly, withholding oxygen is not always the answer.
Higher mortality with low oxygen targets and higher developmental diseases like ROP suggest there is a tradeoff around supplemental oxygen in prematurity. HIFs guide development of blood vessels in the eye, and alveolar development in the lung. Too much oxygen results in blood vessel pruning and insufficient alveolar complexity. On the other hand, too little oxygen interferes with control of pathogens in the gut and predisposes to necrotizing enterocolitis in premature infants. Hypoxia worsens NEC by interfering with gut barrier function, impairing containment of gut pathogens, and exacerbating inflammation that sets off a pathological cascade ending with gut ischemia and necrosis.
A Canadian study last year suggests a Goldilocks approach. Giving intermediate oxygen lowered mortality without increasing complications in preterm infants. Taylor and colleagues assigned centers to intermediate (88–93%) or high (90–95%) saturation targets. A 6-month washout period was applied to sites which switched targets during the study period. 2,739 infants received high oxygen and 6,813 infants were treated with intermediate oxygen. The intermediate group had higher survival without morbidity (adjusted odds ratio [aOR] 1.59; 95% CI: 1.04, 2.45).
Summary: the difficulty of choosing the right oxygen target for premature babies highlights the importance of evolutionary mismatch and tradeoffs in early life oxygen. If inadequate oxygen is given, our youngest patients risk higher mortality and NEC. If they receive too much O2, blindness and permanent lung damage can occur. Follow up studies will be needed to confirm the intermediate approach for premature neonates demonstrated by Taylor and colleagues. However, for babies born at term, meta-analyses suggests that giving air initially during resuscitation instead of 100% oxygen is a superior approach for mortality and morbidity. Interested readers are referred to this excellent review of this topic.
References
Maltepe, E., Saugstad, O. Oxygen in Health and Disease: Regulation of Oxygen Homeostasis-Clinical Implications. Pediatr Res 65, 261–268 (2009). https://doi.org/10.1203/PDR.0b013e31818fc83f
Welsford M, Nishiyama C, Shortt C, Isayama T, Dawson JA, Weiner G, Roehr CC, Wyckoff MH, Rabi Y; International Liaison Committee on Resuscitation Neonatal Life Support Task Force. Room Air for Initiating Term Newborn Resuscitation: A Systematic Review With Meta-analysis. Pediatrics. 2019 Jan;143(1):e20181825. doi: 10.1542/peds.2018-1825.
Askie LM et al. Neonatal Oxygenation Prospective Meta-analysis (NeOProM) Collaboration. Association Between Oxygen Saturation Targeting and Death or Disability in Extremely Preterm Infants in the Neonatal Oxygenation Prospective Meta-analysis Collaboration. JAMA. 2018 Jun 5;319(21):2190-2201. doi: 10.1001/jama.2018.5725.
Taylor RS, Singh B, Mukerji A, Dorling J, Alvaro R, Lodha A, El-Naggar W, Yoon EW, Shah PS; Canadian Neonatal Network Investigators. Intermediate vs. High Oxygen Saturation Targets in Preterm Infants: A National Cohort Study. Neonatology. 2025;122(1):106-113. doi: 10.1159/000540278.
Categories: Uncategorized
Joe Alcock
Emergency Physician, Educator, Researcher, interested in the microbiome, evolution, and medicine
Leave a comment