I explored this topic in a piece I wrote for the Evolution and Medicine Review.
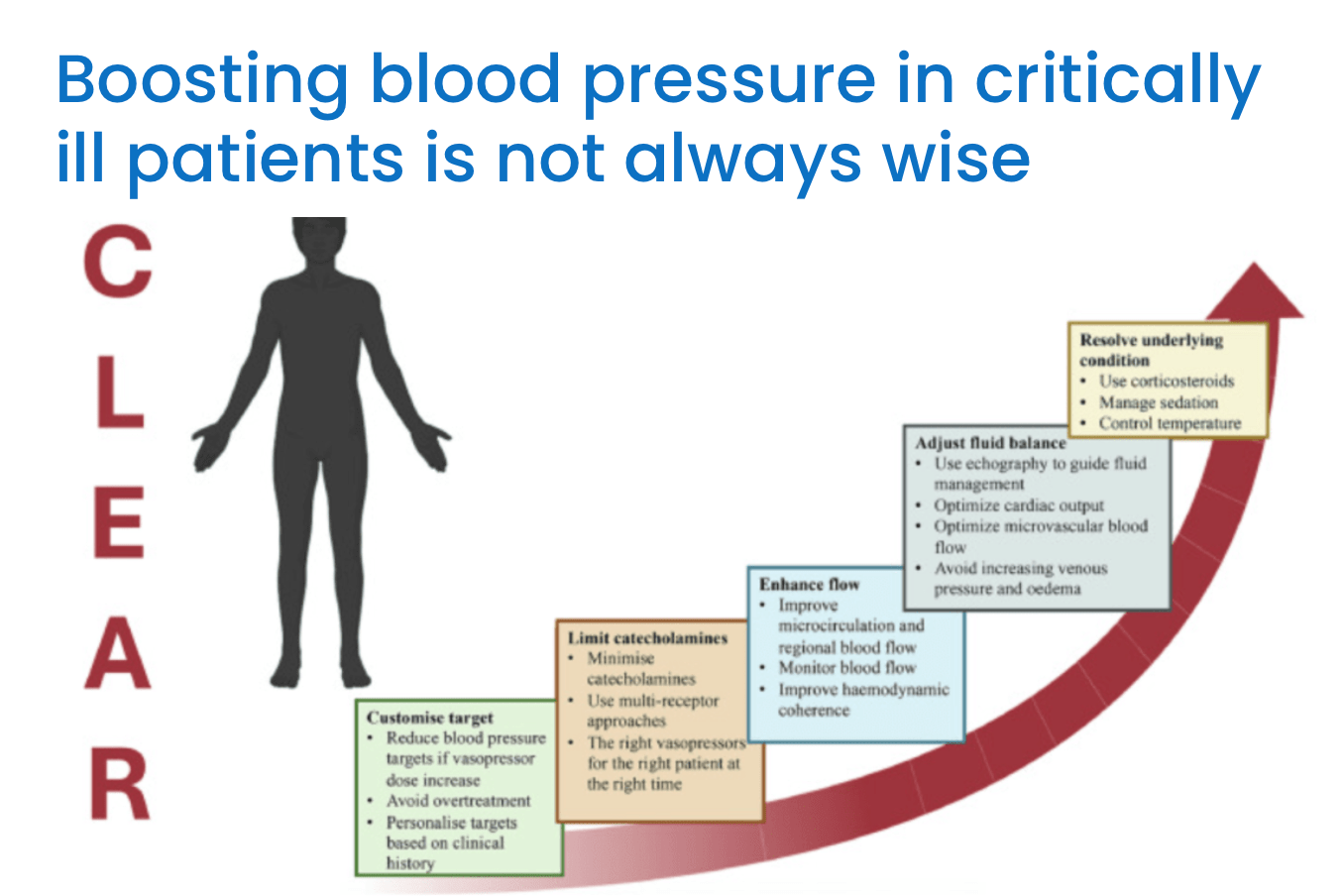
How should we treat critically ill patients who come in with shock? How fast should we intervene and at what blood pressure target? What should we use to raise blood pressure and improve flow? Dozens of research papers have been written on this conundrum, but we (almost) never consider the possibility that low blood pressure might itself be helpful in some patients. In the years since I started medical school, many papers have been published that challenge the conventional wisdom of aggressively treating these patients with fluids and vasopressors. I discuss a few of these in the EvMed Review. The take-away from these studies is not simply that excess fluids can be bad or that vasopressors some with harmful side effects. Taken together, they point to possible benefits for hypotension in some critically ill patients. In other words, sometimes it might be adaptive to have a blood pressure lower than normal.
Categories: Uncategorized
Joe Alcock
Emergency Physician, Educator, Researcher, interested in the microbiome, evolution, and medicine
This is a nice graphic. It’s interesting that the last item in the Resolve box is ‘control temperature’.
That’s right, and I don’t think the authors meant we should try to increase the temperature. There are parts of the CLEAR protocol that I disagree with!